THALIDOMIDE - ORAL
PHONETIC PRONUNCIATION: (tha-LID-oh-mide)
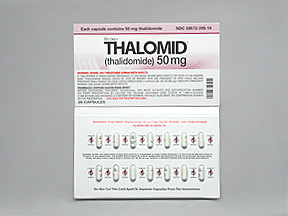
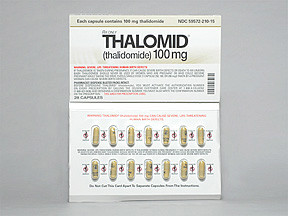
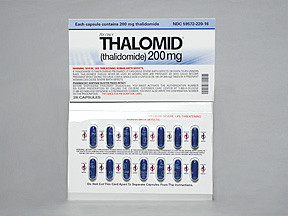
COMMON BRAND NAME(S): Thalomid
GENERIC NAME(S): thalidomide
Uses
USES: This medication is used to treat or prevent certain skin conditions related to Hansen's disease, once known as leprosy (erythema nodosum leprosum). Thalidomide is also used to treat a certain type of cancer (multiple myeloma). It works in Hansen's disease by reducing swelling and redness (inflammation). It also reduces the formation of blood vessels that feed tumors.
How to use THALIDOMIDE - ORAL
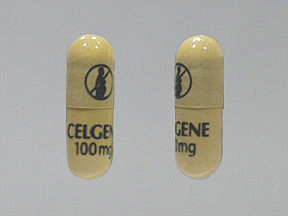
HOW TO USE: Read the Medication Guide provided by your pharmacist before you start using thalidomide and each time you get a refill. If you have any questions, ask your doctor or pharmacist. Take this medication by mouth, usually once daily at bedtime at least 1 hour after the evening meal or as directed by your doctor. Swallow this medication whole with water. Dosage is based on your medical condition and response to treatment. Do not increase your dose or take this medication more often than prescribed. Your condition will not improve any faster, and the risk of serious side effects may be increased. Keep the capsules in their blister pack until ready to use. Do not open or break the capsules, or handle them any more than needed. If any of the powder from the capsule gets on your skin, wash the area with soap and water. Since this drug can be absorbed through the skin and lungs and may harm an unborn baby, women who are pregnant or who may become pregnant should not handle this medication or breathe the dust from broken capsules. All people should wash their hands thoroughly after handling this drug. This medication passes into body fluids (e.g., urine). Avoid contact with body fluids from people taking this drug. Therefore, wear protective clothing (e.g., gloves) when handling these body fluids (e.g., during cleanup). If contact occurs, wash skin with soap and water. Use this medication regularly to get the most benefit from it. To help you remember, take it at the same time each day. If you are taking this medication for Hansen's disease, your skin condition may become worse when the drug is suddenly stopped. Your dose may need to be gradually decreased. Tell your doctor if your condition does not improve or if it worsens after 2 weeks.
Side Effects
Precautions
Interactions
Overdose
Images
Reviews
Faq for THALIDOMIDE - ORAL
Thalidomide Oral is primarily used to treat certain types of cancers such as multiple myeloma and leprosy.
Thalidomide Oral works by inhibiting the growth of abnormal cells in the body and suppressing the production of certain chemicals that cause inflammation.
The common side effects of Thalidomide Oral may include drowsiness, dizziness, constipation, skin rash, nausea, and decreased appetite.
Yes, Thalidomide Oral can have serious side effects such as blood clots, severe skin reactions, nerve damage, birth defects if taken during pregnancy, and a weakened immune system.
Thalidomide Oral should be taken exactly as prescribed by the healthcare provider. It is usually taken once daily or as directed. It should be taken with water and can be taken with or without food.
Yes, Thalidomide Oral may interact with other medications. It is important to inform your healthcare provider about all the medications, supplements, and herbal products you are taking to avoid any potential interactions.
No, Thalidomide Oral should not be taken during pregnancy as it can cause severe birth defects. Female patients must use highly effective contraception methods while taking Thalidomide Oral and for at least 4 weeks after stopping the medication.
The effects of Thalidomide Oral can vary depending on the condition being treated. It may take several weeks or months of continuous treatment to see the desired results.
Thalidomide Oral is not recommended for use in children unless specifically prescribed by a healthcare professional for certain conditions.
Warning
WARNING: Women who are pregnant must not use thalidomide. Women must avoid becoming pregnant while taking this medication. Even a single dose of thalidomide has caused severe (often fatal) birth defects when used during pregnancy. You must have 2 negative pregnancy tests before you start treatment with thalidomide (within 10 to 14 days before and 24 hours before starting), repeating the test at least monthly. Do not start or continue thalidomide treatment unless you have a negative pregnancy test result. Female patients must use 2 effective forms of birth control (or completely avoid sexual intercourse) for 1 month before starting thalidomide, during use, and for 1 month after stopping this drug. Talk to your doctor about reliable birth control choices. If your period is late, or if you have sexual intercourse at any time without using 2 effective forms of birth control, stop taking this medication and contact your doctor right away. (See also Precautions section.) Because thalidomide also passes into semen, men who use this drug and have sex with women must use a latex condom during all sexual contact, even if they have had a vasectomy. Continue using condoms and other birth control as directed until 1 month after thalidomide treatment has been stopped. Only patients who have signed an informed consent and agree to the requirements of the REMS program may obtain and use thalidomide. Only physicians enrolled in REMS may prescribe thalidomide, and only pharmacies enrolled in the program may dispense it. Consult your doctor or pharmacist for more details about the REMS program and for more information about the risks and benefits of using this medication. These requirements apply in the United States. If you live in Canada or any other country, consult your doctor and pharmacist for your country's regulations. When used to treat a certain type of cancer (multiple myeloma), thalidomide can increase the risk of serious blood clots in the legs or lungs, as well as heart attacks and strokes. Seek immediate medical attention if you develop shortness of breath, chest pain, jaw/neck/left arm pain, weakness on one side of your body, slurred speech, sudden vision changes, or arm/leg swelling. While you are taking thalidomide, your doctor may also direct you to take aspirin or other "blood thinners" (e.g., warfarin) to lessen the risk of these types of blood clots. Talk to your doctor for more information, and tell him/her if you have diabetes, high blood pressure or high cholesterol, kidney problems, or if you smoke. (See also Side Effects section.)
Disclaimer
IMPORTANT: HOW TO USE THIS INFORMATION: This is a summary and does NOT have all possible information about this product. This information does not assure that this product is safe, effective, or appropriate for you. This information is not individual medical advice and does not substitute for the advice of your health care professional. Always ask your health care professional for complete information about this product and your specific health needs.
No Reviews Yet